Getting Started
On-Site Pooled Testing
The templates and tools in this section apply to school testing programs where swabs are combined into tubes on-site — or at the school. Separate, individual follow-up tests must be administered to identify any COVID-positive individuals.
What you can find here…
Click to jump to each section about:
Getting Started Checklist
Click here to download our Getting Started Checklist
Vendor Selection:
If using MA DESE Program: Complete district application to DESE & receive match.
If outside of the program, schedule calls with 1-3 vendors to discuss the right program for your school, sign contracts and onboard vendors.
Leads and Training (see Identifying Your Testing Team)
Identify Testing Program Manager for district/program & school leads at each school
Complete trainings from testing service provider
View BinaxNOW training modules #1-4 (note: module 5 isn’t necessary)
Software and Regulatory Onboarding
Using BinaxNOW?
Complete Abbott BinaxNOW Approval Application and Readiness Review Checklist and email to: k12COVID19testing@mass.gov
Complete CLIA Certificate of Waiver for BinaxNOW
Place shipping order (see instructions from DESE email) by filling out the Request Form and email to: COVID19.Resource.Request@mass.gov
Decide who will manage the consenting and outreach for each school and how consents will be organized
Complete software onboarding and trainings with testing service provider (e.g. registering tests for pooling, reflex BinaxNOW, reflex PCR)
Logistics and Supplies
Determine target start date and ensure testing vendor is aware of timeline
Confirm process for handling positive pools (see our Follow-Up Testing Guide)
Document individual follow-up testing method
Set follow-up testing location
Confirm follow-up test outreach leads, follow-up test swabbers, and contact tracing process
Establish and document routine schedule (see our Routine COVID Safety Check Logistics Template)
Identify testing area(s) at each school and document swab collection methods
Confirm process for transporting swabs to lab
Distribute PPE and testing supplies to each school (surgical and N95 masks, eye protection, gloves, gown, hand sanitizer, sanitizing wipes, tissues)
Communications & Consent (See our Communications toolkit)
Create your Three Phase Communications Plan
Schedule initial introductory webinars for school staff & community
Post-Implementation Support
Check out our Peer-to-Peer hub to connect with other schools
Join our virtual pooled testing learning community on facebook.
Monitoring Case Rates
Identify process for monitoring positivity rate on a weekly basis and taking necessary actions to protect the school community
The Shah Family Foundation is available to work with your district or program one-on-one basis to support your pooled testing program. Email us at CovidEdTesting@shahfoundation.org
Identifying your
Testing Team
To support your testing program, it’s important to identify internal, external, or volunteer resources that can take on the responsibilities described in our Identifying Your Testing Team (On-Site Pooled Testing) Guide. One individual can take on multiple roles, and in many cases this is recommended. While school nurses tend to make great candidates, a nursing degree or specialized medical training is not necessary to fulfill any of these roles.
At each school district or program, you need:
Testing Program Manager
At each school, you need:
Testing Coordinator & Software Manager
Pooled Test Observer & Swabber
Follow-Up Test Outreach Lead (not contact tracing)
Follow-Up Test Observer & Swabber
Our Identifying Your Testing Team (On-Site Pooled Testing) Guide contains detailed descriptions of each role.
Example: How Watertown Public Schools staffed their on-site pooled testing program
Deciding on a Follow-Up Testing Protocol
When a pooled test comes back positive, each person in the pool will need to be individually tested to determine who in the pool is COVID-positive.
The goal of individual follow-up testing is to identify and isolate the positive individual(s). When you have tested everyone in the pool and have identified at least one positive, your individual follow-up testing is a success!
The different ways schools have managed follow-up testing for on-site pooled testing are documented in our Follow-Up Testing Guide.
Setting Your Testing Schedule
Your testing schedule will depend on your in-person learning model (everyday, hybrid, etc.). Our weekly testing logistics template can help you think through when each step in the testing process will happen for each group of students. Download our Weekly Testing Logistics Template to help document your school’s process.
A few helpful things to keep in mind when setting your testing schedule
Any trained staff member can administer or observe the test; it does not need to be administered by a healthcare professional. Students in grades 2 and above can swab themselves under observation
Anyone observing a student or staff member self-administering the test should maintain a six-foot distance and wear a face mask and gloves. Anyone administering the test for a student should wear an N95, gown, gloves, and protective eyewear
Testing is quick! It takes less than 30 seconds per student
Turnaround time for pooled test results is 24-36 hours from when samples arrive at the lab. Your testing service provider can provide more specifics
According to the Department of Health and Human Services, individuals in positive pools may maintain their regular schedules, as long as they are scheduled for individual follow-up tests as soon as possible (DESE FAQ, see question #39)
Choosing your swab collection and individual follow-up testing methods are important considerations
Example: Watertown Public Schools Weekly Testing Logistics
Choosing Swab Collection Methods
The on-site Pooled Testing is performed via an anterior nasal swab (“short swab”) that is quick, easy, and painless to administer. This is a gentle, lower-nostril swab – it is not the deep brain-poking swab. Swabbing is quick! It only takes a few seconds per student. Many school districts have reported they can collect swabs from a whole class in 3-5 minutes.
Grades 1 & under & students with disabilities: staff member swabs
Students grade 1 and below and some students with disabilities will have their noses swabbed by a trained staff member. It is recommended that staff doing the swab collection have an N95 or higher respirator, eye protection, gloves, and a gown.
Click here to view our Swab Collection Best Practices for Young Learners and Students with Disabilities.
Grades 2-12 & staff: self swab
Adults and students grade 2 and above can swab their own noses under observation by a trained staff member. Staff observing self-collection should wear a surgical mask and maintain six feet of distance. There are different models for how to organize swab collection. Many school districts and programs use multiple models depending on schedules, school setup, and age / abilities of students.
Here are three swab collection models used by Watertown Public Schools
There are different models for how to organize swab collection. Many schools use multiple models depending on schedules, school setup, and age / abilities of students, and schools are constantly coming up with new ideas for swab collection. Our peer-to-peer hub is a great place to connect with other schools doing Pooled Testing to brainstorm ideas !
Method A (High School)
Student testing at front door station as they arrive; tested in random pools
8:00am - 8:30am
Lunch Time: Pooled Testing for late arriving students
Staff
1 trained observer monitors swabbing
1 additional staff member records names on spreadsheet and matches to tube by scanning barcode
Testing Rate
180 students can be swabbed in the 30 minute morning period.
STEP 1
Staff record name on spreadsheet and scans barcode on tube
STEP 2
Student self-swabs under observation and places swab in tube
STEP 3
Student sanitizes hands and goes to class
Why this method?
Watertown used to test high school students at lunch, but they didn’t always show up. The testing team found it was more reliable and easier to test students as they arrive in the AM; it also gets samples out the door to the lab earlier in the day. Because high school students don’t attend classes in dedicated pods (they mix between classes), the pools do not need to be the same each week. Testing in random pools requires a staff member to scan barcodes to record who is in each pool.
Method B (Middle School)
Student testing at mask break; tests grouped by classroom
10:00am - 11:00am
Tubes are pre-labeled by classroom
Staff
1 trained observer monitors swabbing
Testing Rate
Swabbing takes a matter of seconds per student
STEP 1
Students line up by class
STEP 2
Student self-swabs under observation and places swab in tube
STEP 3
Student sanitizes hands and goes outdoors for a mask break
Why this method?
Middle-schoolers attend class in dedicated pods, so their test groups should stay the same each week. Most middle-school students can swab their own noses. The testing team found it was most efficient to have students self-swab at a testing station on their way out the door for a mask break. This way the testing didn’t interfere with instructional time and could be conducted outside.
Method C (Elementary School):
Student testing in school hallway; tests grouped by classroom
9:00am - 11am
Tubes are pre-labeled by classroom
Staff Needed:
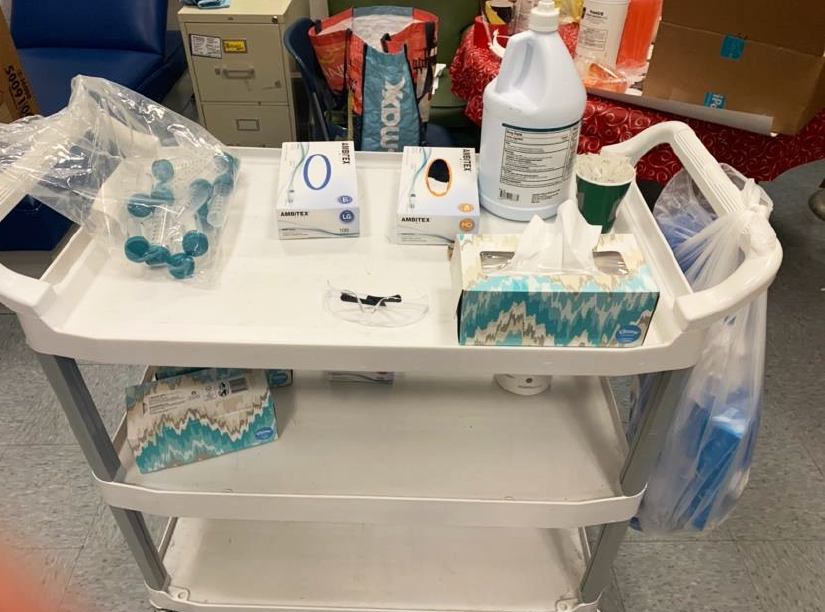
1 trained staff member travels corridors with a cart, stopping outside each classroom
Testing Rate:
3-5 minutes per classroom.
STEP 1
Cart arrives outside of classroom. Students signed up for testing come into the hallway and line up
STEP 2
One by one, students self-swab under observation and place swab in tube. Grades 2+ self-swab; grades K-1 may require assistance
STEP 3
Student sanitizes hands and goes to class
Why this method?
Elementary school students are grouped by learning pod, so groups should stay the same each week. In addition, many students at this level need assistance swabbing themselves. Watertown found that it was quickest and easiest to have nurses travel the corridors with a testing cart, stopping by each classroom for 3-5 minutes to take samples.
Keeping School Personnel Safe During Testing
Anterior nasal swabs and saliva tests are not considered to be aerosol generating procedures, but PPE is recommended for people administering or observing the tests simply because, at times, they need to be close to the individual being tested.
In this section we describe the types of PPE recommended for personnel involved in testing.
Personnel actively collecting swabs:
Fitted* N95 or higher respirator (though a surgical mask can be used if a N95 is not available)
Eye protection
Gloves
Gown
*during the public health emergency, and with the wide variety of N95 respirators in use, it is not always possible to perform fit testing. Nurses and health care staff are encouraged to conduct a user seal check to determine if the respirator is being properly worn and should be performed with each use. The user seal check procedure is described here.
Personnel observing swab collection
surgical mask
gloves
All personnel and students should maintain 6 feet of distance and wear masks during swab collection. Any and all staff who are not actively involved in testing should maintain 6 ft of distance and wear masks.
Getting Your Pools To The Lab
All pooled tests must be sent to a testing lab for analysis. Your testing service provider will provide options for getting your pools to the lab, which may include overnight shipping or courier service.
The options for vendors in the current DESE Program are described below. Please check with your testing service provider for preferred methods and how shipping costs are billed.
For districts working with CIC Health or Project Beacon
How to get swab to the Broad Institute (Located in Cambridge)
Option 1: School employee / volunteer drives pools to the lab.
Option 2: Arrange for a courier service - your testing provider can help you identify an approved courier service.
Option 3: Use FedEx, UPS, or another shipping/logistics provider.
When to get pools to the Broad Institute
The earlier the better. It is strongly recommended that pools arrive before 1pm on testing day for fastest turnaround time (potentially same-day results)
Please note: Quick Start Package pools for CIC Health are delivered to CIC Health Office (One Broadway, Cambridge, MA). All future pools are delivered to the Broad.
For districts working with Ginkgo
How to get pools to Ginkgo (Located in the Seaport District of Boston)
Option 1: Ginkgo will provide a prepaid, pre-addressed FedEx shipping label.
Option 2: Ginkgo will help you arrange courier service.
When to get pools to Ginkgo
Ginkgo’s lab operates 24 hours a day and can process pools upon arrival. Results take 24-48 hours.
Districts using FedEx should schedule a pickup in time for next-day delivery (the cutoff is usually around 4pm-5pm).
Identifying and Isolating Positive Cases
It’s tempting to view finding a positive case as a failure. That is NOT the case. Finding a positive case means your testing program is working. Isolating that positive case means that you have made your school safer for everyone.
See our section on Positive Pools & Communications for details about how to handle this stage in the process.
See the following section on Close Contacts and Other Public Health Guidance to determine how to manage positive pools and positive individuals.
Individuals who have a positive result on an individual test will need to be isolated as defined in the DESE Protocols for Responding to COVID-19.
Note. For Early Education Providers in Massachusetts, please refer to the COVID-19 Child Care Playbook from the Massachusetts Department of Early Education and Care for specific public health guidance for your COVID-19 testing program.
Close Contacts and Other Public Health Guidance
Note. For Early Education Providers in Massachusetts, please refer to the COVID-19 Child Care Playbook from the Massachusetts Department of Early Education and Care for specific public health guidance for your COVID-19 testing program.
In Between a Positive Pool Result and an Individual Positive
Students who are part of a positive pool do not need to quarantine while they await their follow-up test results, unless they are symptomatic. Symptomatic students should follow the DESE Protocols for Responding to COVID-19. If not symptomatic, individuals in a positive pool will often return to school for follow-up testing. These individuals do not have to quarantine and can ride on buses or take their normal transportation method to school, as long as they are not symptomatic.
Individuals who receive positive, follow-up individual test results will need to be isolated as defined in the DESE Protocols for Responding to COVID-19.
For details on how to communicate with individuals in a positive pool, please see our section on Positive Pools & Communications.
Contact Tracing
There are many different models for contact tracing being deployed in Massachusetts schools. It is important to be in close contact with your local board of health to determine what role the school will play vs. the local board of health. Statewide contact tracing resources are also available via the Massachusetts Community Tracing Collaborative will reach out to provide support to those individuals, work to identify close contacts, and reach out to them. When talking with your local board of health, you can reference various resources including from the Massachusetts Department of Public Health and the Massachusetts Association of Health Boards.
Defining Close Contacts
The Massachusetts Department of Public Health defines close contacts as
Being within 6 feet of a COVID-19 case (someone who has tested positive) for a cumulative total of 10-15 minutes during a day while the person was infectious.
Infectious period – Symptomatic Individual: Begins 48 hours prior to symptom onset, and while they were symptomatic
Infectious period – Asymptomatic Individual: Begins 48 hours prior to the collection of their positive test,* until anytime in the 10 days after the test.
Having direct contact with infectious secretions of a COVID-19 case while not wearing PPE.
Being in the same room as an individual if you are consistently separated by 6 feet of distance does not meet the definition of a close contact.
*The date of the pooled test should be used to determine the beginning of the infectious period.
Quarantining Close Contacts
Local boards of health are best positioned to provide advice on quarantine requirements for individual cases. The CDC suggests that close contacts quarantine for:
With testing: At least 7 days, provided that all of the following are satisfied: they are tested (PCR or antigen) on day 5 or later from their last exposure to the positive individual and receive a negative result, they have not experienced any symptoms, and they conduct active monitoring for symptoms through day 14. CDC estimates that this strategy is 95% effective.
Without testing: At least 10 days, provided that all of the following are satisfied: they have not experienced any symptoms and they conduct active symptom monitoring through day 14.
With symptoms OR without symptom monitoring: At least 14 days. This applies to anyone who has experienced symptoms, even if they have a negative test, and to those who are unable to conduct active symptom monitoring
Returning To School After a Positive COVID-19 Test
When individuals exit quarantine, they must continue masking and complying with other safety measures. If a student or staff member has a positive test result, they will need to stay in self-isolation for at least 10 days and until at least 24 hours have passed with no fever and improvement in symptoms, without the use of fever reducing medications.
Getting Started Templates and Examples
SOPs, Best Practices, and Schedule Plans for Swab Collection
Template:
Guide: Follow-Up Testing Guide
Case Study: Case study: Watertown Public Schools